Key points
- The 2025-2026 COVID vaccine is approved only for people aged 65 and older and those at high risk for serious complications.
- High-risk individuals include those aged 65+, pregnant, immunocompromised, or with chronic conditions such as asthma, diabetes, and obesity.
- People under 65 without high-risk conditions can get vaccinated via a doctor’s prescription, living in a state with expanded pharmacist authority, or paying out of pocket.
- Several states have taken independent action to expand vaccine access in response to the federal government's scaled-back access.

In fall 2025, getting a COVID-19 vaccine has become significantly more complicated. For the first time since the vaccines were introduced, the Centers for Disease Control and Prevention (CDC) and the Food and Drug Administration (FDA) are no longer recommending universal vaccination. Access now depends on age, health status, where you live, and how your state is responding to new federal guidance.
If you're trying to decide whether you or your child should get vaccinated this year, here's what to know about eligibility, risk, insurance coverage, and what to do if you want the shot but aren't sure how to get it.
Who is eligible for the COVID-19 vaccine in 2025?
The new FDA guidelines
In August 2025, the FDA approved three updated COVID-19 vaccines targeting the LP.8.1 strain:
- Pfizer-BioNTech: Approved for ages 5 and up
- Moderna (monovalent, LP.8.1 strain): Approved for ages 6 months and older
- Novavax: Approved for ages 12 and older
However, approval alone doesn’t guarantee access. In September, the CDC’s Advisory Committee on Immunization Practices (ACIP) abandoned its previous universal recommendation for everyone 6 months and older. Instead, the panel unanimously endorsed an "individual-based decision-making" approach.
This means COVID-19 vaccination is now a personal health choice, ideally made in consultation with your doctor—especially if you're between 6 months and 64 years old.
Vaccination is still recommended for people:
- 65 and older
- With underlying health conditions that increase the risk of severe COVID-19
What qualifies as a high-risk condition?
According to the CDC, these include:
- Asthma or other lung conditions
- Heart disease
- Diabetes (Type 1 and 2)
- Obesity
- Cancer
- Chronic kidney or liver disease
- Immunocompromised states (e.g., HIV, transplant)
- Pregnancy
- Depression and other mental health conditions
- Neurological conditions (e.g., dementia)
- Smoking (current or former)
- Sedentary lifestyle or physical inactivity
The FDA estimates that between 100 million and 200 million Americans meet one or more of these risk criteria.
Can healthy people still get the shot?
Technically, yes — but it’s not simple. If you don't meet the FDA's or CDC's criteria for increased risk, you're still allowed to get the vaccine. However, you may face obstacles, such as:
- Pharmacies unwilling to administer it without clear CDC recommendation
- Doctors who are hesitant to prescribe it "off label"
- Insurance companies that may not cover the cost for low-risk individuals
Still, no federal policy currently prevents healthy people from getting vaccinated. The shot is still FDA-approved, and providers can choose to offer it.
Why was the COVID vaccine policy changed this year?
A shift in philosophy: From public health to personal choice
The federal government’s rationale centers on two ideas:
- Widespread natural and vaccine-induced immunity
- Evolving virus patterns and shifting public demand
In short, they argue that the U.S. population has enough immunity from past infections and prior vaccinations that an annual booster is no longer needed for everyone. Instead, the focus is shifting to those most vulnerable to severe illness.
Medical community pushback
The policy shift has drawn criticism from more than 75 major medical organizations, including:
- American Academy of Pediatrics (AAP)
- American College of Obstetricians and Gynecologists (ACOG)
- American Pharmacists Association (APhA)
- American Public Health Association (APHA)
These groups argue that:
- Removing the universal recommendation creates confusion
- At-risk patients may fall through the cracks
- Limiting access undermines public health goals
ACIP rejects prescription requirement but ends universal recommendation
At its September 2025 meeting, ACIP took two important votes:
- They rejected a proposal to require prescriptions for the COVID-19 vaccine. This preserves access in many states where pharmacists can vaccinate without a doctor's order.
- They voted to abandon universal recommendations for COVID vaccines. Instead, the new approach is "shared clinical decision-making" for everyone under 65.
This middle-ground position means you can still get vaccinated if you want to—but you may need to be more proactive, and access will vary widely depending on where you live.
What are states doing to expand access?
Because ACIP guidance influences pharmacy laws in many states, some states have stepped in with their own policies to maintain vaccine availability.
States that have taken action include:
- California, Oregon, Washington: Created the West Coast Health Alliance to publish unified vaccine guidance and maintain access
- New York, New Jersey, Connecticut: Issued executive orders or directives to preserve pharmacist authority
- Colorado, Illinois, Arizona: Directed state agencies to issue standing orders for vaccine access
- Virginia, Minnesota, Nevada, New Mexico, Pennsylvania: Took regulatory steps to authorize COVID vaccinations outside ACIP guidance
In these states, you may be able to self-attest to eligibility or get vaccinated without a formal prescription.
How can I get the COVID vaccine if I’m not in a high-risk group?
You still have options:
1. Doctor’s office or hospital
- Many providers are offering the vaccine "off label"
- A conversation with your doctor may be enough—no written prescription required
2. Participating pharmacies
- Some states allow pharmacists to administer based on FDA approval, even without CDC recommendation
- Call ahead or check the pharmacy website for eligibility criteria
3. Out-of-pocket payment
- If insurance won’t cover the shot, you can pay directly
- Cost ranges from $150 to $200 depending on provider and location
Will insurance cover the 2025 COVID vaccine?
Yes, in most cases.
Despite ACIP’s softened stance, most insurers say they will continue covering COVID vaccines through at least 2026:
- Medicare: Will cover for those 65+ based on its own guidelines
- Medicaid and CHIP: Federal officials say coverage will remain in place
- Marketplace and private plans: Industry group AHIP says coverage will be honored regardless of ACIP's vote
What to watch out for:
- Out-of-network providers may charge full price
- Some pharmacies may not process insurance for non-recommended vaccines
If you're unsure, contact your insurer or provider directly.
What about children and pregnant women?
Children
- Moderna is approved for ages 6 months and older
- Pfizer is approved for ages 5 and up
- Novavax is approved for 12 and older
However, because ACIP no longer officially recommends the vaccine for healthy children, some pharmacies may not offer it without a prescription or self-attestation of risk.
The AAP still recommends vaccination for:
- All children 6 to 23 months
- All children 2 to 18 years who have not been previously immunized
Pregnancy
- The FDA lists pregnancy as a high-risk condition, so access is technically permitted
- ACIP deferred its decision on formal pregnancy recommendations
- ACOG continues to recommend COVID-19 vaccination during pregnancy to protect both parent and baby
If you're pregnant, speak with your OB-GYN about the benefits and risks. Most providers continue to offer the vaccine during pregnancy.
What should I do next?
1. Check your risk status
- You may qualify based on a broad list of underlying conditions
2. Talk to your doctor
- They can advise on your personal risk and whether vaccination is a good option for you or your child
3. Know your state’s rules
- In some places, pharmacists can vaccinate without a prescription
- In others, you may need to go through your doctor
4. Confirm insurance coverage
- Call your insurer to understand whether the vaccine is covered for your situation
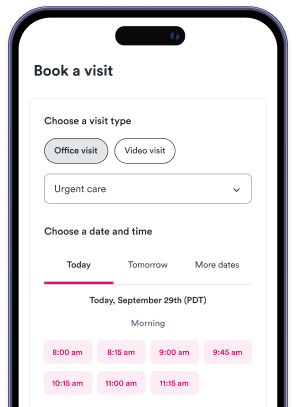
5. Use Solv to find a provider
- Solv helps you locate urgent care clinics and telehealth providers that can consult on vaccine eligibility and administer COVID shots where available
Final thoughts
In 2025, COVID vaccine access has shifted from a public health mandate to a matter of personal and provider judgment. While the shots are still widely available, the rules vary by state, by pharmacy, and by insurance plan.
Most importantly, vaccination remains a powerful tool to reduce your risk of serious illness—especially if you’re pregnant, over 65, or living with a chronic health condition. If you want the shot this year, you'll likely still be able to get it. It just may take a little more planning.
FAQs
Who is eligible for the COVID-19 vaccine in 2025?
In 2025, the COVID-19 vaccine is approved for people aged 65 and older and those considered high-risk for serious complications. This includes individuals with conditions such as pregnancy, immunocompromised states, chronic conditions like asthma, diabetes, obesity, chronic kidney or liver disease, heart conditions, HIV, neurological conditions, depression and other mental health conditions, smoking or history of smoking, and a sedentary lifestyle or physical inactivity.
Can healthy people under 65 years old still get the COVID-19 vaccine?
Yes, healthy individuals under 65 can still get the vaccine, but it's not straightforward. They would need to receive a doctor’s prescription, live in a state that has issued a standing order or expanded pharmacist authority, and be willing to pay out of pocket if their insurance doesn’t cover it.
Why was the COVID-19 vaccine policy changed in 2025?
The policy was changed due to widespread natural and vaccine-induced immunity. After five years of global exposure and multiple rounds of vaccination, many Americans have some level of protection. The new strategy prioritizes “science, safety, and common sense,” arguing that healthy individuals may not benefit significantly from yearly boosters.
How can I get the COVID-19 vaccine if I’m not eligible under federal guidance?
There are a few options. You can get a prescription from your doctor, look for a state with expanded access, or pay out of pocket. However, some providers may be hesitant to prescribe the vaccine due to liability concerns, appointments may be hard to secure during seasonal surges, and pharmacies in 19 states are required to follow CDC guidance and may decline to administer the shot, even with a prescription.
Will my insurance cover the COVID-19 vaccine in 2025?
It depends on your plan and your state. Under the Affordable Care Act, insurance providers are required to cover vaccines that are recommended by the CDC’s Advisory Committee on Immunization Practices (ACIP). However, because ACIP has not issued formal recommendations for the 2025 COVID vaccine, coverage is now discretionary. Some states have explicitly directed insurers to cover the vaccine regardless of CDC guidance.





![Accident Prone: Common Holiday Accidents [INFOGRAPHIC]](https://ucl-cdn-prod.thirdparty.solvhealth.com/dir/media/W1siZiIsIjIwMTMvMTAvMjYvMTBfNTJfMTRfMjQ1X2hvbGlkYXlfYWNjaWRlbnRzLnBuZyJdLFsicCIsInRodW1iIiwiMzAweCJdXQ?sha=ace44d1b024a1586)